Although it’s a normal part of the aging process, degenerative disc disease can cause painful symptoms. Fortunately, there are minimally invasive treatment options that help provide relief and keep you active.
What Is Degenerative Disc Disease (DDD)?
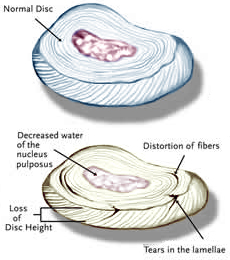
Degenerative disc disease (DDD) is part of the natural process of growing older. As we age, our intervertebral discs lose their flexibility, elasticity, and shock absorbing characteristics. The outer fibers that surround the disc, called the annulus fibrosis, become brittle and are more easily torn. At the same time, the soft gel-like center of the disc, called the nucleus pulposus, starts to dry out and shrink. The combination of damage to the intervertebral discs, the development of bone spurs and the gradual thickening of the ligaments that support the spine can all contribute to degenerative arthritis of the lumbar spine.
To a certain degree, this process happens to everyone. However, not everyone who has degenerative changes in their lumbar spine has pain. Many people who have “normal” backs have MRIs that show disc herniations, degenerative changes, and narrowed spinal canals. Every patient is different, and it is important to realize that not everyone develops symptoms as a result of degenerative disc disease.
What Are The Symptoms Of Degenerative Disc Disease?
When degenerative disc disease becomes painful or symptomatic, it can cause several different symptoms due to the compression of the nerve roots. Depending on where your degenerative disc is located, it could cause:
- Back pain
- Radiating leg pain
- Neck pain
- Radiating arm pain
These symptoms are caused by the fact that worn out discs are a source of pain because they do not function as well as they once did, and as they shrink, the space available for the nerve roots also shrinks. As the discs between the intervertebral bodies start to wear out, the entire lumbar spine becomes less flexible. The result can be back pain and stiffness, especially towards the end of the day.
How Is Degenerative Disc Disease Diagnosed?
The diagnosis of degenerative disc disease begins with a complete physical examination. A spine specialist will examine your back for flexibility, range of motion, and the presence of certain signs that suggest your nerve roots are being affected by degenerative changes in your back. This often involves testing the strength of your muscles and your reflexes to make sure that they are still working normally. You will often be asked to fill out a diagram that asks you where your symptoms of pain, numbness, tingling and weakness are occurring.
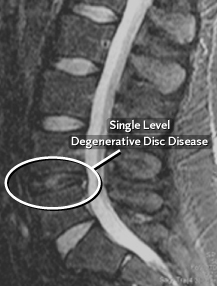
A series of x-rays is also usually ordered for a patient with back pain. If degenerative disc disease is present, the x-rays will often show a narrowing of the spaces between the vertebral bodies, which indicates the disc has become very thin or has collapsed. Bone spurs also can form around the edges of the vertebral bodies and also around the edges of the facet joints in the spine. These bone spurs can be seen on an x-ray, and are also called osteophytes. As the disc collapses and bone spurs form, the space available for the nerve roots starts to shrink. The nerve roots exit the spinal canal through a bony tunnel called the neural foramen, and it is at this point that the nerve roots are especially vulnerable to compression.
In many situations, doctors will order a MRI or a CT scan (CAT scan) to evaluate the degenerative changes in the lumbar spine more completely. A MRI is very useful for determining where disc herniations have occurred and where the nerve roots are being compressed. A CT scan is often used to evaluate the bony anatomy in the spine, which can show how much space is available for the nerve roots and within the neural foramina and spinal canal.
How Is Degenerative Disc Disease Treated?
It is best to see a spine specialist who will discuss with you the treatment options appropriate for your diagnosis. For most people who do not have evidence of nerve root compression with muscle weakness, conservative, non-surgical therapies, such as medication, rest, exercise and physical therapy, are typically recommended.
Surgery is offered only after conservative treatment has have failed to adequately relieve the symptoms of pain, numbness and weakness over a significant period of time.
The benefits of spine surgery, however, must be weighed against the risks. Your surgeon will be able to discuss the risks and benefits of surgery with you, and the likely results of operative versus non-operative treatment.
